

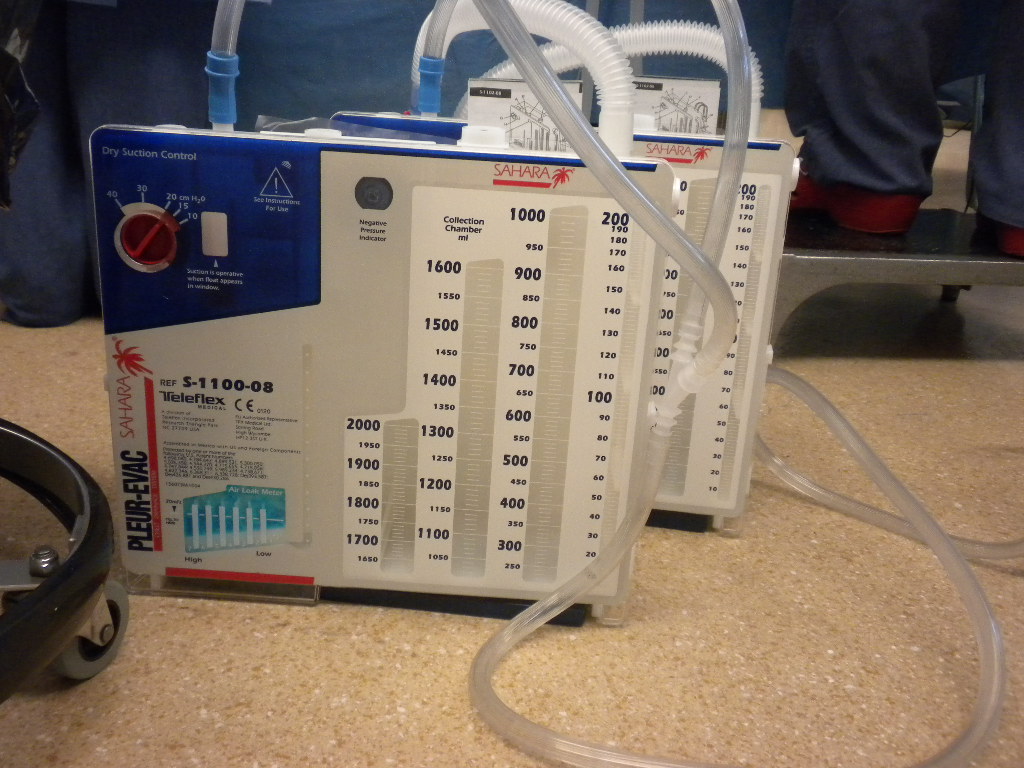
SET UP INSTRUCTIONS If suction is prescribed, follow steps 1 through 5. Use only a standard luer slip tip syringe to fill the Air Leak Meter. The clamp on the patient tube should be placed away from the patient, avoiding accidental clo&re. Follow hospital policy regarding the use of protective wear. Caution should be used when the possibility exists for exposure to blood or body fluids. CAUTIONS Keep the Pleur-evac Sahara System below the patient’s chest level at all times. Stripping with the clamps closed can result in the build-up of excessive positive pressure. Stripping of the thoracic tubing must be done with the thoracic tubing clamp open. In the event of an air leak, clamping chest tubes could lead to a tension pneumothorax. Chest tubes should not be clamped except when changing Pleur-evac Sahara System. The collected contents of the Pleur-evac Sahara Chest Drainage System should not be used for reinfusion. L INDICATIONS FOR USE The Pleur-evac Sahara Chest Drainage System is indicated: + To evacuate air and/or fluid from the chest cavity or mediastinum + To help prevent air and/or fluid from reaccumulating in the chest cavity or mediastinum + To help re-establish and maintain normal intrathoracic pressure gradients + To facilitate complete lung re-expansion to restore normal breathing dynamics 1. These instructions will address the set-up and operation of the Pleur-evac Sahara Chest Drainage System and the Autotransfusion Bag. By attaching the Pleur-evac Sahara Autotransfusion Bag, the Pleur-evac Sahara Chest Drainage System serves as a collection/reinfusion system for autologous WARNINGS DISPOSAL blood. PRODUCT DESCRIPTION The SaharaTM Chest Drainage System is provided as a sterile, non-pyrogenic unit intended for single patient use. CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician. volume and mode of ventilation.Deknatel Product Group SURGICAL PRODUCTS D’ ’ ONE SINGLE USE UNIT DO NOT RESTERILIZE STERILE: Contents sterile unless package has been opened or damaged. If exhaled tidal volumes are less than 75% of inhaled tidal volumes, evaluate and consider changes in tidal volume, frequency, PEEP, inspiratory time, pressure vs.Maintain pH between 7.25 and 7.45 by adjusting the rate.consider FiO 2 adjustments to maintain saturations between 88% – 95%.
After careful consideration of initial settings

Hess and Kacmarek (2019) suggest the following for ventilator management in patients with air leaks. Permissive hypercapnia and permissive hypoxemia (PaO 2 > 50 mm Hg) should be considered. Higher FiO 2 may be used lieu of higher pressures. Plateau pressures should be minimized, kept below 28 cm H 2 O and driving pressure less than 15 cm H 2 O. Tidal volumes should be set from 4-8 mL/kg PBW with an inspiratory time between 0.5-0.8 sec. Additionally, frequent adjustments of cycling criteria may be needed, as well as, trigger sensitivity since suction pressure of the chest tube may trigger the ventilator. Use of pressure support should be used cautiously, as inspiration only terminates when flow is decreased to a certain level and the ventilator may not cycle appropriately if the leak is greater than this level. An air leak may also increase with spontaneous breathing. Some patients may need paralysis to reduce air leak and maintain acceptable cardiopulmonary function. Leak compensation should be turned off with PAL. volume should carefully be considered in determining which mode best minimizes the leak. While pressure control ventilation (PCV) controls peak pressures, caution must be used as it may increase the leak, as it maintains the higher pressure throughout the inspiratory phase of the cycle. cited a case study that demonstrated volume loss through a fistula increased from 15% to 54% with the addition of 15 cm H 2 O PEEP. This will work to minimize peak airway pressure (Paw). To reduce the leak, both inspiratory pressure and PEEP need to be minimized. The challenge and goal for mechanical ventilation management becomes aimed at techniques to minimize the pressure gradient across the fistula, reduce the leak and allow healing to occur. When secondary to barotrauma or direct lung injury, mortality has been reported from 50-60%. PALs can be identified by either an intermittent (during inspiration) or continuous air leak through a chest tube.Īir leaks in mechanically ventilated patients are associated with an increase in morbidity and mortality. It can occur from trauma, surgery, vascular line placement, tumors, or from specific diseases, including, but not limited to, COPD and ARDS. Most commonly, it can be seen as a pneumothorax, subcutaneous emphysema, pneumomediastinum, or pneumopericardium. Extra-alveolar air can come in many different forms.


 0 kommentar(er)
0 kommentar(er)
